Definition:- An Anal fissure or Rectal Fissure is a break or tear in the skin of the anal canal
Description:- Anal fissures may be noticed by bright red anal bleeding on toilet paper, sometimes in the toilet. If acute they may cause pain after defecation but with chronic fissures pain intensity is often less. Anal fissures usually extend from the anal opening and are usually located posteriorly in the relatively unsupported nature and poor perfusion of the anal wall in that location. Fissure depth may be superficial or sometimes down to the underlying sphinter muscle.
Causes :-
Most anal fissures are caused by STRETCHING of the mucosa beyond its capability
The most common cause of non healing is spamming of the internal anal sphincter of the internal anal sphincter muscle which results in impaired blood supply to the anal mucosa.
Other common causes of anal fissures include; Childbirth trauma in women Crohn’s Disease Ulcerative Colitis
Epidemiology:- The incidence of anal fissure is around 1 in 350 adults. They occur equally commonly in men and women and most often occur in adults aged 15 to 40
Prevention:- For Adults;
Avoiding straining when defecation,
Careful anal hygiene after defection,
In case of pre-existing or suspected fissure, use of a lubricating ointment,
In infants, frequent diaper change can prevent anal fissure
Treatment:- Non- surgical treatment are recommended initially for acute and choric anal fissures. These include topical Nitroglycerin or calcium channel blockers or injection of Butulinum toxin into the anal sphincter
Other measures include warm Sitz baths, topical anesthetics, high fiber diet and stool softerners
Medication:-
Local application of medication to relax the sphincter muscle, thus allowing the healing to proceed, with Nitroglycerine ointment
Calcium channel blocker with Nifedipine ointment
A combined surgical and pharmacological treatment, administered by colorectal surgeons, is direct injection of Botulinum toxin(Botox) into the anal sphincter to relax it.
Surgery:-
1) Lateral internal sphincterotomy
2) Anal dilation
3) Stretching
DEFINITION
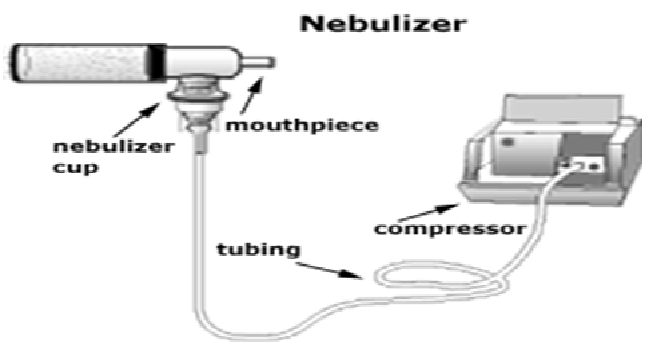
Nebulization is the process of medication administration via inhalation. It utilizes a nebulizer which transports medications to the lungs by means of mist inhalation.
INDICATION
Nebulization therapy is used to deliver medications along the respiratory tract and is indicated to various respiratory problems and diseases such as:
• Broncho-spasms
• Chest tightness
• Excessive and thick mucus secretions
• Respiratory congestions
• Pneumonia
CONTRAINDICATIONS
In some cases, nebulization is restricted or avoided due to possible untoward results or rather decreased effectiveness such as:
• Patients with unstable and increased blood pressure
• Individuals with cardiac irritability (may result to dysrhythmias)
• Persons with increased pulses
• Unconscious patients (inhalation may be done via mask but the therapeutic effect may be significantly low)
EQUIPMENTS
• Nebulizer and nebulizer connecting tubes
• Compressor oxygen tank
• Mouthpiece/mask
• Respiratory medication to be administered
• Normal saline solution
PROCEDURE
1. Position the patient appropriately, allowing optimal ventilation.
2. Assess and record breath sounds, respiratory status, pulse rate and other significant respiratory functions.
3. Teach patient the proper way of inhalation:
o Slow inhalation through the mouth via the mouthpiece
o Short pause after the inspiration
o Slow and complete exhalation
o Some resting breaths before another deep inhalation
4. Prepare equipments at hand
5. Check doctor’s orders for the medication, prepare thereafter
6. Place the medication in the nebulizer while adding the amount of saline solution ordered
7. Attach the nebulizer to the compressed gas source
8. Attach the connecting tubes and mouthpiece to the nebulizer
9. Turn the machine on (notice the mist produced by the nebulizer)
10. Offer the nebulizer to the patient, offer assistance until he is able to perform proper inhalation (if unable to hold the nebulizer [pediatric/geriatric/special cases], replace the mouthpiece with mask.
COMPLICATIONS
Possible effects and reactions after nebulization therapy are as follows:
• Palpitations
• Tremors
• Tachycardia
• Headache
• Nausea
• Broncho-spasms (too much ventilation may result or exacerbate Broncho-spasms)
• TEACHINGS
As nurses, it is important that we teach the patients the proper way of doing the therapy to facilitate effective results and prevent complications (demonstration is very useful). Emphasize compliance to therapy and to report untoward symptoms immediately for apposite intervention.
Auscultatory gap is the temporary disappearance of sounds normally heard over the brachial artery when the cuff pressure is high and the reappearance of the sounds at a lower level.
Provide excellent clues to the physiological functioning of the body.
• Alterations in body flexion are reflected in the body temp, pulse, respirations and blood pressure.
• These data provide part of the baseline info from which plan of care is developed.
• Any change from normal is considered to be an indication of the person’s state of health.
Author:PINKY CHOUDHARY
Description :- Placenta Previa
Definition :- Its is type of ante-partum hemorrhage. When the placenta is implanted partially or completely over the lower uterine segment , it is called Placenta previa.
Etiology :-
(1) The exact cause of implantation of placenta is unknown .
(2) Dropping Down Theory
(3) Persistence of chorionic activity in deciduas capsularis
(4) Big surface area of placenta
(5) Multiparity
(6) Increase maternal age
(7) History of previous cessarion section or scar in uterus
(8) Prior curettage use
Types :- There are four types of placenta previa .
(1) Type 1st( low lying ) – Major part of placenta is attached to upper segment & only margin reach on to lower segment but not up to os.
(2) Type 2nd (marginal ) – Placenta reach to margin of internal os but doesn’t cover it .
(3) Type 3rd ( Incomplete or partial central ) – Placenta cover the internal os partially .
(4) Type 4th (central or total ) – Placenta completely cover the internal os .
Clinical Features :- (1) Vaginal Bleeding
(2) Bleeding painless
(3)Bleeding is causeless & recurrent
(4) Anemic due to visible blood loss
Diagnosis :- –Sonography
–Magnetic resonance imaging
Management :- The following guidelines are useful to minimize the risk-
-Adequate antenatal care
– Antenatal diagnosis
– Significance of “Warning Hemorrhage ‘’ should not be ignored
Management at home :-
-Patients is immediately put to bed .
-To assess the blood loss .
-Note the pulse ,BP , & degree of anemia .
-Quick gentle abdominal examination .
-Vaginal examination must not be done .
Management in hospital :-
-Treatment depend on duration of pregnancy, fetal & maternal status & extend of hemorrhage .
-To give advice to pts for supplement therapy .
– Encourage the pts for steroid therapy .
– Vaginal delivery would be considered only in type 1& 2 placenta previa .
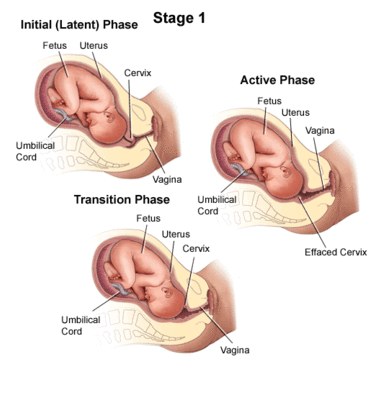
Definition:- Labour is called prolonged when the combined duration of first and second stage is more than 18 hours.
Labour is considered prolonged when cervical dialation rate is less than 1cm/hr.
Cause:-
a. First Stage:- Failure to dilate cervix
-Fault in power (abnormal uterine contraction)
-Fault in passage (contracted pelvis)
-Fault in passenger.
-Other (injudious admn. of analgesic)
b. Second Stage:-
-non descend of presenting part is due to failure in power( inability in bearing down, uterine inertia, epidural analgesia, constriction ring), fault in passage , fault in passenger.
Diagnosis:- prolonged labour has not diagnosis but it can be manifestated as abnormal. The cause of this prolonged labour can be detected by abdominal and vaginal examination.
First Stage:- first stage is considered prolonged when duration is more than 12 hrs. The rate of cervical dilatation is less than 1cm/hr in a primi and less than 1.5cm/hr in multi.
Second stage :- second stage is considered as prolonged when it is more than 2hrs in primi and more than 1hr in multi.
Diagnosis features are :-
Sluggish descending of presenting part
Variable degrees of moulding and caput formation in cephalic presentation.
Management:-
Prevention:- Antenatal or early intra-natal detection of the factors which produce prolonged labour.
Use of partograph, help early detection.
Selective and judicious augmentation of labour.
Change of posture in labour other than supine to increase uterine contraction
When progress is slow attempt should be made to determine the cause before deciding on management for insufficient uterine action is to encourage ambulation to produce normal activity.
The upright position for mother improve the application of the presenting part on to the cervix,this would make the contractions less painful but stronger and more efficient.
Adequate analgesic should be given to mother.
All observation are to be recorded on partogram.
The mother should be encouraged to empty the bladder about 2hrly.
Feotal Heart rate should be monitored.
Jishu Baiju
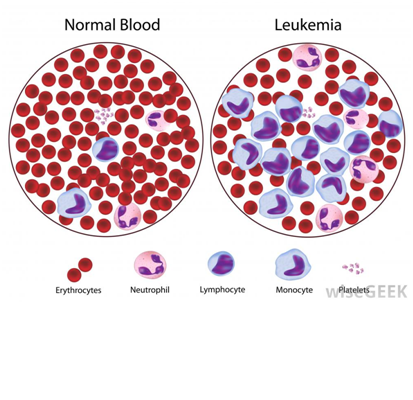
Description: – Leukemia ( Blood Cancer)
Definition: – It is a neoplastic proliferation of one particular cell l type and also affecting the bone morrow & lymphoid system which are all known as hematological neoplasm.
Increased white blood cells is called as Blast cells.
The term leukemia refers to an increase level of leukocytes in the circulation.
Etiology:- 1. Genetic factor(Abnoemal chromosomalmay increase the risk for leukemia such as down syndrome or trisomy 21.)
2. HTLV-I (The presence of primary immune deficiency &infection with the Human T-
lymphocyte Virus Type-I)
3. Exposure to chemical & benzene
4. Exposure to radiation
5. Smoking
6. Chemotherapy or Radiation
Classification: It is clinically submitted into a variety of large group.
A. Acute Leukemia: It is characterized by the rapid increase of immature blood cells. This crowding makes the bone marrow unable to produce healthy blood Cells. The result is a massive accumulation of immature, nonfunctional cells or blast in the bone marrow & in the other Organ.
B. chronic Leukemia: It is distinguish by the excessive build up of relatively mature but still abnormal wbc taking the month or years to progress.
BONE MARROW forming cell
Sign & Symptom:-
A. Aneamia
B. Seizures
C. Headache
D. Spleenomegaly
E. Bleeding
F. Fever
G. Weight loss
H. Fatigue
I. Sweating
J. Abdominal Pain
K. Joint Pain
L. Tiny Red Spot on Skin
Diagnostic Findings:-
A.Bone marrow biopsy
B.Cytogenetics
C.PCR( Polymer chain Reaction)
D.Lumber Puncture ( Spinal Tab )
E.CBC
F. FNAC( Fine Needle Aspiration Cytology)
Treatment:-
A.Chemotherapy
B.Drug:- Doxorubicin, Cisplastin. Monoclonal Antibodies, Interferon Alpha ,Rituximab
C.Radiation Therapy
D. Blood Transfusion
E. Bone marrow transplantation
F. stem cell transplantation
G.Interferon Alpha Therapy With or Without chemotherapy
H. Use of specific Tyrosin kinase Inhibitotrs
Tarun Mudgul
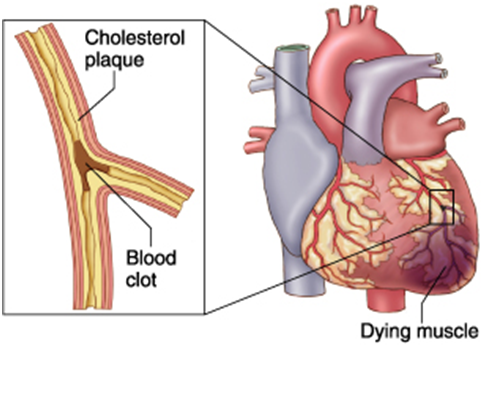
Definition :- MI is a cardio vascular diseases in which it is a life threatening condition characterized by the form of localized necrosis area within the myocardium usually caused reduced blood flow in a coronary artery.
INCIDENCE:- Each year US nearly 1 million people have MI and ¼ of these people dies from MI.
ETIOLOGY:- There are many causes or risk factors of MI:-
Ischemia, atherosclerosis, smoking, spasm of coronary artery, hypotension, aneamia.
Pathophysiology :-
Due to any etiological factors & Artherosclerosis
Inflammatory response
↓
Formation of lumen in vessels
↓
Narrowing of vessels
↓
Obsrruction in vessels
↓
Decrease in blood flow
↓
Rupture & haemorrhage into plaque
↓
Thrombous formation
↓
Ischemia
↓
Sudden cardiac death & MI
Clinical Features :- According to systems –
(1) Cardiovascular System –severe chest pain
–Discomfort
–palpitation
–Elevated B.P.
–Pulse Deficit
–Cardiogenic shock
(2)Respiratory Tract System –Dyspnea
–Shortness of breath
–Tachypnea
_ Pulmonary edema
(2) Gastro –intestinal Tract — Nausea & vomiting
(3) Genitourinary Tract _ Decrease urinary output
(4) Skin- _cool , pale appearance
(5) Neurological – —Anxiety
—Reastlessness
—Light headache
—Visual disturbance
—Altered speech
Diagnosis :-
(1) History collection about –smoking , alcoholism
–previous medical illness
(2) Physical examination —Inspection of skin( pale colour )
—Level of consciousness
(2) ECG ( Electro Cardio Graph )
(3) CBC (Complete Blood Count )
(4) Blood glucose level
(5) MRI (Magnetic Resonance Imaging )
(6) Serum Myoglobin & tropenin (protein found in myocardium)
Immediate / Emergency Managemant :-
–Ensure patients airway
–Administer oxygen therapy
–Provide IV fluid therapy
–Determine location & medicated for pain
–Obtain ECG & cardiac enzyme level
–Assess the need of thrombolytic therapy
–Monitor vital sign & prepare for CPR
Medical Management :–
(1) Administer Antiplatelets agents Example –Asprin , Ticlopidine
(2) Administer Beta –Blockers Example – Atenolol Timolol
(3) Administer Calcium – Channel Blockers Example – Nimodipine , Foledipine
(4) Administer Analgesic drug as per as docters order .
(5) Administer Cholesterol lowering agents .
(6) Administer Thrombolytic Therapy. Example :- Heparin
(7) Administer ACE ( Angiotenssive Converting Enzyme ) . Example- Captopril
Surgical Management :-
(1) PTCA (Percutaneous Transluminal Coronary Angioplasty ) :- A ballon catheter inserted into the heart , in the blocked coronary artery is entered . The ballon on the catheter is inflated this procedure compress the plaque against the wall of artery this restoring the opening of artery .
(2) Coronary Atberectomy :- It is the removal of plaque from the coronary artery .
(3) Coronary Artery Bypass Graft :- Grafting of blocker of coronary artery .
Nursing Management :-
—Assess the condition of the patients .
—-Provide comfortable position & ventilation to the patients .
—-Monitor vital signs & diagnostic test .
—-Teach about to take low fat or cholesterol diet .
—- To teach about the stop smoking & alcoholism .
—-Teach about to maintain personal hygienic condition .
—- Maintain I/O chart of patient .
—-To give health education regarding the dietary pattern & healthy life style.
—-Instruct to avoid lifting of heavy load & heavy exercise .
—- Teach the client to avoid stressful condition .
—-Adm. the drug as per as physician orders .
—-Provide psychological support .
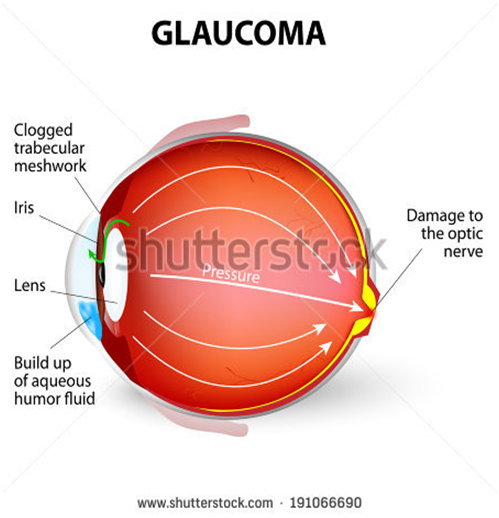
Glaucoma refers to a group of disorders that lead to damage to the optic nerve, due to the increased fluid pressure in the eye. The optic nerve carries visual information from the eye to the brain .Damage to the optic nerve causes vision loss.
TYPES: there are 4 types of glaucoma-
1- Open angle or chronic glaucoma
2- Close angle or acute glaucoma
3- Congenital glaucoma
4- Secondary glaucoma
ETIOLOGY AND RISK FACTOR – Family history of glaucoma ,older age, diabetes, cardiovascular disease, migraine, myopia, eye trauma, prolong use of corticosteroids
PATHOPHYSIOLOGY- Due to the etiology and risk factors (emotional stress , illness, long term corticosteroids)
Turns structural alterations in the aqueous outflow system
It leads to functional alteration condition such as increased intra ocular pressure
Than due to the alteration of the function ,the optic nerve damage
When the arophy of an optic nerve
Visual loss.
CLINICAL MANIFESTATIONS-
1 chronic or open angle glaucoma
Visual impairement
Blurring visin
Mildly aching eyes
2 close or acute angle glaucoma
Severe eye pain
Red eye deceased or cloudy visin
Swelling of the eye
Pupil doesn’t react to light
Headache
Nausea and vomiting
3 congenital glaucoma
Tearing
Sensitivity to light
Red eye
Enlarge ment of one eye or baoth eye
Cloudyness of the front of the eye
DIAGNOSTIC TEST –
1 Tonometry- this test is used to measures the intra ocular pressure.
Normal intra ocular pressure ranges from 10 to 21 mmhg.
2 slit lamp examination –this test is used for see the effect of glaucoma on the anterior eye structure including the cornea , iris, and lens.
3 opthalamoscopy – this test is for facilitates visualization of fundus.
MEDICAL MANAGEMENT-
Epinephrine , mannitol(osmotic diuretic) , isosorbide (to reduce the effect of blood glucose level)
SURGICAL MANAGE MENT-
Trabeculectomy
Iridectomy
Filtering procedure
NURSING DIAGNOSIS-
RISK FOR BLINDNESS FROM EXTREMELY HIGH INTRA OCCULAR PRESSURE CAN BE ADDERESSED AS A COLLABORATIVE PROBLEMS.
RISK FOR INEFFECTIVE THERAPEUTIC REGIMEN MANAGEMENT RELATED TO COMPLEX MEDICATION SHEDULE.
ANXIETY RELATED TO FEAR OF BLIND NESS NAD HOSPITALIZATION.
PAIN REALATED TO SURGERY.
NUTRITION DEFICIENCY RELATED TO SURGERY.
Keywords:
Increased intra occular pressure,
Optic nerve damage,
Open angle glaucoma(chronic),
Close angle glaucoma(acute),
Congenital,
Secondary,
Management (medical and nursing),
DESCRIPTION-
The uterus is not a fixed organ. Minor variation in position in any direction occurs constantly with changes in posture, with straining, with full bladder or loaded rectum. Only when the uterus rests habitually in a position beyond the limit of normal variation, should it be called displacement.
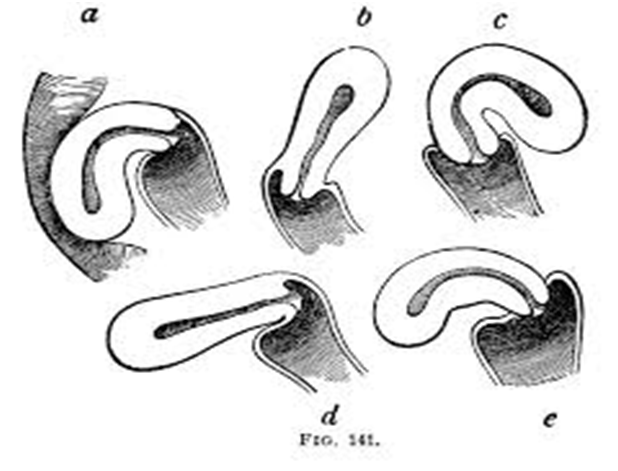
RETROVERSION-
Definition-retroversion is the term used when the long axes of the corpus and cervix are in line and the whole organ turns backwards in relation to the long axis of the birth canal.
RETROFLEXION-
Retroflexion signifies a bending backwards of the corpus on the cervix at the level of internal os. The two conditions are usually present together and are loosely called retroversion or retrodisplacement.
DEGREES-
Conventionally, three degrees are-
FIRST DEGREE- The fundus is vertical and pointing towards the sacral promontory.
SECOND DEGREE- The fundus lies in the sacral hollow but not below the internal os.
THIRD DEGREE- The fundus lies below the level of the internal os.
CAUSES-
1]DEVELOPMENTAL
2]ACQUIRED
DEVELOPMENTAL
Retrodisplacement is quite common in fetuses and young children. Due to developmental defect, there is lack of tone of the uterine muscles. The infantile position is retained. This is often associated with short vagina with shallow anterior vaginal fornix.
ACQUIRED
1] PUERPERAL-
The stretched ligaments caused by childbirth fail to keep the uterus in its normal position. A subinvoluted bulky uterus aggravates the condition.
2] PROLAPSE
Retroversion is usually implicated in the pathophysiology of prolapsed which is mechanically caused by traction following cystocele .
3] TUMOR
Fibroid, either in the anterior or posterior wall produces heaviness of the uterus and hence it falls behind.
4] PELVIC ADHESION
Adhesions either inflammatory, operative or due to pelvic endometriosis pull the uterus posteriorly.
INCIDENCE
Retroversion is present in about 15-20% of normal women.
CLINICAL PRESENTION
1] Chronic premenstrual pelvic pain
2] Backache
3] Dyspareunia
4] Infertility
DIAGNOSIS
1] Bimanual examination
2] Speculum examination
3] Rectal Examination
The retrodisplacement may be confused with hard faecal mass in the rectum, small fibroid on the posterior wall of the uterus and small ovarian cyst in the pouch of Douglas.
PREVENTION
1] To empty the bladder regularly
2] To increase the tone of the pelvic muscles by regular exercise.
3] To encourage lying in prone position for half to one hour once or twice daily between 2 to 4 weeks postpartum.
COORECTIVE TREATMENT
1] PESSARY
2] SURGICAL
PESSARY-Use of pessary is almost obsolete in present day obstetric/gynecological practice.
Usually HODGE- SMITH Pessary is used. The pessary acts by stretching the uterosacral ligaments so as pull the cervix backwords.
SURGICAL TREATMENT
The principle of surgical correction is ventro suspension of the uterus by plicating the round ligaments of both the sides extra peritoneally to the under surface of the anterior rectus sheath .
This will pull the uterus forwards and maintains it permanently.
Haemoglobin Formation.
Description: – It is the red, oxygen carrying pigment in the RBCs. It consist of the protein globin united with the pigment haem.
The Iron in the haem the ferrous form. Each ferrous combines loosely and reversibly with one molecules of oxygen.
There are 4 haem to the one molecules of haemoglobin, contains 4 iron atoms and can carry 4 molecules of oxygen.
Molecular weight of haemoglobin is 68,000.
SOME IMPORTANT DEFINITION:-
1. Oxyhaemoglobin:- Haemoglobin react with oxygen to form oxyhaemoglobin and is represented as HbO2.
2. Carbamino –Haemoglobin:- Carbon dioxide reacts with haemoglobin to form carbamino-haemoglobin.
3. Reduced Haemoglobin:- Haemoglobin from which oxygen has removed.
4. Carboxy Heamoglobin:- Carbon Monoxide reacts with Haemoglobin to form carboxy haemoglobin.
5. Methaemoglobin:- When either reduced or oxygenated haemoglobin is exposed to various drugs to various drugs or oxidizing agents ,the ferrous is oxidized to ferric form and the compound is called methaemoglobin.
NORMAL VALUES:
1. At birth 23gm/dl, because RBC count s more.
2. At the end of 3 month 10.5gm/dl
3. Adults:
Males :- 14-18gm/dl
FemaleS:- 12-15.5gm/dl
FUNCTIONS:-
1. Transport of oxygen from lungs to tissues.
2. Transport of CO2 from the tissues to the lungs.
3. It acts as an excellent acid base buffer,being a protein.
SYNTHESIS:-
Synthesis of haemoglobin requires the provision of nutrients e.g. proteins ,vitamins.
It only takes place in the developing RBCs.
FACTORS CONTROLLING HAEMOGLOBIN FORMATION:-
1. Role of proteins:- It helps in globin formation.
2. Role of minerals:- IRON – It helps in formation of haem. COPPER, COBALT AND CALCIUM – helps in the absorption ,mobilization and utilization of iron.
VARIETIES OF HAEMOGLOBIN:-
Adult haemoglobin
Foetal heamoglobin:- Its structure is same as of HBA, except that the beta chains are replaced by gamma
JISHU BAIJU
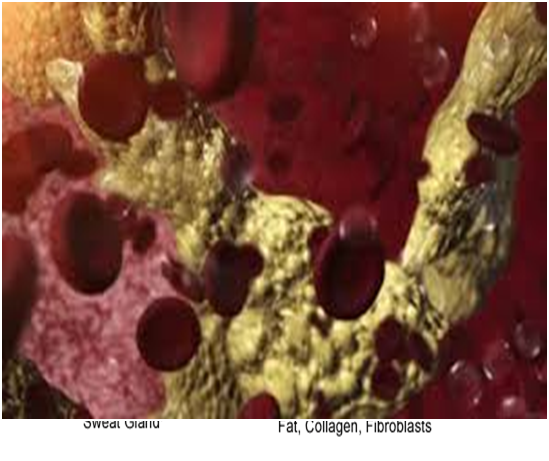
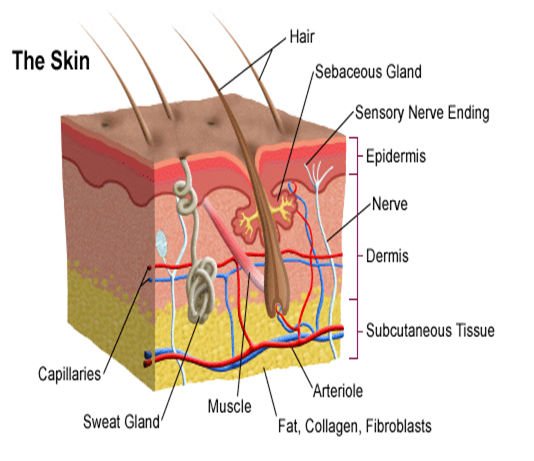
Description: SKIN: – The skin is the continuation of the membranous lining the body openings. It contains glands, hair, nails and consists of two layers.
1. Epidermis
2. Dermis
EPIDERMIS:- The outer skin:-
It is the most superficial layer of the skin and made up of stratified epithelium. It is thickest on the palms of the hands and soles of feet. It contains no blood vessels and nerve cells and its nutrition is derived from the capillaries of the dermis. The Epidermis consists of five layers:
1. Stratum corneum:- It is the most superficial layer and it is made up of dead and highly Keratinised cells.
2. Stratum lucidum:- It is made up of clear non granulated cells.
3. Stratum granulosum:- It consist of granular cells and is about three cells layer thick.
4. Stratum spinosum:- It is 3-5 cells thick layers. The individual cells have a prickly appearance due to the fact that cytoplasmic processes come out from each cell to meet their fellow cytoplasmic strands.
5. Stratum germinativum :- It is the deepest layer of epidermis, made up of columnar cells which give rise to the new cells. It also contains melanocytes which synthesize a pigment called melanin.
DERMIS:- It is a thick and tough elastic layer of connective tissues which supports the hair.
1. Hair :- The hair develops from the hair follicles located in the epidermis.The part of the hair above is the shaft and the remainder ,the root. The colour of the hair depends on the amount of melanin pigment.
The Arrector pilli muscle is attached to the hair follicle.
2. Sebacious glands :- They develops from the hair follicles and usually open into it but in the face they may open into the exterior directly. They are most numerous in the skin of the scalp.
The secretion of the sebaceous glands is rich in oily substances that keep the hair soft.
3. Sweat glands: – They are basically a highly coiled tubular structure in the deeper part of the dermis. Sweat is synthesized by the coiled portion of the sweat glands from water, salt urea and other waste products. Two types of sweat glands are recognized: – Apocrine sweat glands and Ecrine sweat glands.
FUNCTIONS:-
1. PROTECTIVE FUNCTION:- Ultra violet rays of sun i.e. light rays less than 360 um in wavelength can cause damage to the skin producing sun burn and cancer of skin , called ultra violet radiation injury.
2. SENSE PERCEPTION:- Skin provides a sensory covering over the entire body.It contain nerve ending as well as various receptors for general sensation such as touch, pain, pressure and temperature.
3. TEMPERATURE REGULATION:- The different organs of the body by way of metabolism generate large quantities of heat which reaches the skin via blood .
4. WATER BALANCE:- The first layer of epidermis is such a membrane that it does not allow water to pass in and out.
5. Skin helps to eliminate waste products such as urea in the sweat.
JISHU BAIJU