DEFINITION: Ulcerative Colitis is the inflammation that affects the lining of the large intestine.
CAUSES: – Genetic factor
– Auto immune disorder
– Environmental factor
– Diet & breast feeding
PATHOPHYSIOLOGY: ulcerative colitis affects the superficial mucosa of the colon
It becomes edematous and inflamed
The disease process usually begin in rectum
The bowel narrow, shortness and thicker
Obstruction, perforation and bleeding
Ulcerative Colitis
SIGNS AND SYMPTOMS:
• Abdominal pain, nausea, vomiting, and fever
• Rectal Bleeding
• Eye Lesions
• Anorexia
• Anemia
• Dehydration
• Weight Loss
DIAGNOSIS:
Blood test
Imaging
• Ultrasound
• Computed tomography
• Magnetic resonance imaging
• X–Ray
• Endoscopy
• Colonoscopy
MANAGEMENT:
Medical management:
Medication are dependent on severity, disease location and complication.
1. Sedative Drugs
2. Anti- Diarrheal
3. Antibiotics
4. Corticosteroids
5. Immunodulators
Nutritional Therapy: Suggest about oral fluid, high protein diet with supplement vitamin therapy and iron replacement.
Control Pain and Diarrhea
Avoid cold foods and smoking.
Surgical management:
1. Total Colectomy with ileostomy:
The surgical creation of an opening into the ileum or small intestine allowed drainage of fecal matter from the ileum to the outside of body.
2. Total Colostomy with continent ileostomy:
The removal of entire colon this procedure eleminance the need and external fecal collection bag.
3. Total Colostomy with ileonal anastomosis:
The total colostomy with ileonal anastomosis
Nursing Management:
Patient in community settings or those recently diagnosed may primarily require education about diet, medication and referral to support group.
For Hospitalized Patients:
1. Parental Nutrition
2. Fluid Replacement
3. Physical care
4. Psychological Support
Nursing Diagnosis:
1. Diarrhea related to inflammation process.
2. Acute pain related to increased peristalsis and gastro-intestinal inflammation.
3. Fluid Volume Deficit related to anorexia, nausea and diarrhea.
4. Imbalanced Nutrition less than body requirement related to dietary restrictions.
5. Impaired Skin Integrity related to malnutrition.
6. Activity intolerance related to fatigue.
7. Knowledge deficit related to disease conditions.
Description
Normally, an egg and sperm are fertilized inside a woman’s uterus. If the fertilized egg attaches to the lining of the uterus and continues to grow, a baby is born about 9 months later. This process is called natural or unassisted conception.
IVF is a form of Assisted Reproductive Technology (ART). This means special medical techniques are used to help a woman become pregnant.
There are five basic steps to IVF:
Step 1: Stimulation, also called super ovulation
• Medicines, called fertility drugs, are given to the woman to boost egg production.
Step 2: Egg retrieval
• A surgery, called follicular aspiration, is done to remove the eggs from the woman’s body.
• The health care provider inserts a thin needle through the vagina and into the ovary and sacs (follicles) containing the eggs. The needle is connected to a suction device, which pulls the eggs and fluid out of each follicle, one at a time.
• The procedure is repeated for the other ovary.
Step 3: Insemination and Fertilization
• The man’s sperm is placed together with the best quality eggs. The mixing of the sperm and egg is called insemination.
• Eggs and sperm are then stored in an environmentally controlled chamber. The sperm most often enters (fertilizes) an egg a few hours after insemination.
Step 4: Embryo culture
• When the fertilized egg divides, it becomes an embryo. Laboratory staff will regularly check the embryo to make sure it is growing properly.
Step 5: Embryo transfer
• Embryos are placed into the woman’s womb 3 – 5 days after egg retrieval and fertilization.
• The procedure is done in the doctor’s office while the woman is awake. The doctor inserts a thin tube (catheter) containing the embryos into the woman’s vagina, through the cervix, and up into the womb. If an embryo sticks to (implants) in the lining of the womb and grows, pregnancy results.
• Unused embryos may be frozen and implanted or donated at a later date.
DEFINITION: Pancreatitis is the inflammation of pancreas.
TYPES: Pancreatitis is divided into two types:
• Acute
• Chronic
CAUSES: – Long term use of alcohol
-Bacterial or viral infection
-Auto immune problems
– Gall stones
– Injuries to the pancreas
PATHOPHYSIOLOGY:
Due to the above causes
Self digestion of pancreas by its own proteolitic enzyme
Gall stone enter the common bile duct
Obstructing the flow of pancreatic juice
Activating the powerful enzyme within the pancreas
Leads to vasodilatation, increased vascular permeability, necrosis, erosion Pancreatitis
SIGNS AND SYMPTOMS:
• Abdominal pain, nausea, vomiting, and fever
• Diaphoresis
• Hypotension
• Cyanosis
• Weight loss
• Tachycardia
• Hyperglycemia
• Respiratory distress
DIAGNOSIS:
Blood
Imaging
• Ultrasound
• Computed tomography
• Magnetic resonance imaging
• X–Ray
ERCP(Endoscopic retrograde choliangio pancreatography)
MANAGEMENT:
An acute attack of pancreatitis usually lasts a few days. An acute attack of pancreatitis caused by gallstones may require removal of the gallbladder or surgery of the bile duct. After the gallstones are removed and the inflammation goes away, the pancreas usually returns to normal.
Treatment for chronic pancreatitis
Chronic pancreatitis can be difficult to treat. Doctors will try to relieve the patient’s pain and improve the nutrition problems. Patients are generally given pancreatic enzymes and may need insulin. A low-fat diet may also help.
Surgery may be done in some cases to help relieve abdominal pain, restore drainage of pancreatic enzymes or hormones, treat chronic pancreatitis caused by blockage of the pancreatic duct, or reduce the frequency of attacks.
Patients must stop smoking and drinking alcoholic beverages, follow their doctor’s and dietitians dietary advice.
Maintain fluid volume and prevent renal failure.
COMPLICATIONS
Early complications include shock, infection, systemic inflammatory response syndrome, low blood calcium, high blood glucose, and dehydration. Blood loss, dehydration, and fluid leaking into the abdominal cavity (ascites) can lead to kidney failure. Respiratory complications are often severe. Pleural effusion is usually present. Shallow breathing from pain can lead to lung collapse.
INTRODUCTION:- snoring is the vibration of respiratory structure and the resulting sound, due to obstructed air movement during breathing while sleeping. In some cases the sound may be loud and unpleasant. Snoring during sleep may be a sign, or first alarm of obstructive sleep apnea (OSA). Researchers say that snoring is a factor of sleep deprivation
CAUSES:- Generally speaking the structures involved are the uvule and soft palate. The irregular airflow is caused by a passageway blockage and is usually due to the following:-
Throat weakness, causing the throat to close during sleep.
Mispositioned jaw, often caused by tension in the muscles.
Fat gathering in and around the throat.
Obstruction in the nasal passageway.
Obstructive sleep apnea.
The tissues at the top of airway touching each other, causing vibration.
Relaxants such as alcohol or other drugs relaxing throat muscles.
Sleeping on one’s back, which may result in the tongue dropping to the back of the mouth
IMPACT:- Snoring is known to cause sleep deprivation to snore and those around them, as well as daytime drowsiness, irritability, lack of focus and decreased libido. It can cause significant psychological and social damage to sufferers. Multiple studies reveal a positive correlation between loud snoring and risk of heart attack (about +34% chance) and stroke (about + 67% chance)
PREVALENCE:- Statistics on snoring are often contradictory, but at least 30% of adults and perhaps as many as 50% of people in some demographics snore. One survey of 5713 American residence identified habitual snoring in 24% of men and 13.8% of women. This suggests an increased susceptibility to snoring as age increase.
TREATMENT:- Almost all treatment for snoring revolve are as following :-
Clearing the blockage in the breathing passage.
Advised to lose weight (to stop fat from pressing on the throat)
Stop smoking ( smoking weakens and clogs the throat)
Sleep on their side (to prevent the tongue from blocking the throat)
OTHER TREATMENT:- Nasal sprays, Nasal strips or Nasal clips, lubricating sprays, oral appliances and “ANTI-SNORE” clothing and pillow, to such unusual activities as playing the didgeridoo.
Description:- What is mental health? Describe components, criteria, indicators and characteristics of mental health.
It is a state of balance between the individual and the surrounding world, a state of harmony between oneself and others ,co-existence between the realities of the self and that of other people and the environment.
Definitions:- Karl Menninger defines mental health as an adjustment of human beings to the world and to each other with a maximum of effectiveness and happiness.
Components :-
1. The Ability to accept self:- A mentally healthy individual feels comfortable about himself.
2. The capacity to feel right towards others:-An individual who enjoys good mental health is able to be sincerely interested in others welfare.
3. The ability to fulfill life task:- The third important component of mental health is bestows on an individuals the ability to meet the demand of life.
Criteria:-
a. Adequate contact with reality
b. Control o9f thought and imagination
c. Efficiency in work and play
d. Social acceptance
e. Positively self concept
f. A healthy emotional life
INDICATORS:-
1. A positive attitude towards self
2. Growth, deve4lopment and the ability for self actualization
3. Integration
4. Autonomy
5. Perception of reality
6. Environmental mastery
CHARACTERISTICS:-
a. He has an ability to make an adjustment
b. He has a sense of personal wealth
c. He solves his problems largely by his own efforts
d. He has a sense of responsibility
e. He can give and accept love
f. He lives in world of reality rather than fantasy
g. He shows emotional maturity in his behavior
h. He has developed a philosophy of life that gives meaning and purpose to his daily activities
i. He has a variety of interest and generally lives a well balanced life of work, rest and recreation
INTRODCATION:-The umbilical cord or Funnies extend from the fetus to the placenta & transmit the umbilical cord vessels which are two arteries & one vein. These are enclosed& protected by gelatinous substance which known as Wharton’ Jelly which form from the mesoderm.
Structure of umbilical cord:-
(1) Covering Epithelium:- It is lined by a single layer of amniotic membrane or amniotic epithelium.
(2) Wharton s jelly :-It consist of elongated cells in a gelatinous substance , it has got protected function to the umbilical cord .
(3) Blood vessels :- Initially there are four vessels–Two veins
–Two arteries
The arteries are derived from the internal iliac arteries of the fetus & carry the venous blood from the fetus to the placenta . The two umbilical veins, the right one is disapper by the four month of pregnancy. Leaving behind one vein which carries blood from the placenta to the fetus .
Characteristics:- It is about 50 cm in length with an usual variation 30-100 cm with variation of 1-2.5 cm . It shows a spiral twist from the left & right from as early as 12 weeks due to spiral turn taken by the vessels , vein around the arteries.
Anatomical variations of the umbilical cord:-
(1) Succenturiate lobe of placenta:- A small extra lobe is present , separate from the main placenta & join to it by blood vessels that run through the membrane to reach it. The danger is that this small lobe may be retain in uterus after the placenta is delivered or born . If it is not remove , it may leave to infection & hemorrhage. The nurse must examine every placenta for identify of a retain lobe of placenta in uterus.
(2) Circumvallates placenta
(3) Battledore insertion of the cord
(4) Velamentius insertion of the cord
(5) Bipartile placenta
(6) Tripartile placenta
Definition:- An Anal fissure or Rectal Fissure is a break or tear in the skin of the anal canal
Description:- Anal fissures may be noticed by bright red anal bleeding on toilet paper, sometimes in the toilet. If acute they may cause pain after defecation but with chronic fissures pain intensity is often less. Anal fissures usually extend from the anal opening and are usually located posteriorly in the relatively unsupported nature and poor perfusion of the anal wall in that location. Fissure depth may be superficial or sometimes down to the underlying sphinter muscle.
Causes :-
Most anal fissures are caused by STRETCHING of the mucosa beyond its capability
The most common cause of non healing is spamming of the internal anal sphincter of the internal anal sphincter muscle which results in impaired blood supply to the anal mucosa.
Other common causes of anal fissures include; Childbirth trauma in women Crohn’s Disease Ulcerative Colitis
Epidemiology:- The incidence of anal fissure is around 1 in 350 adults. They occur equally commonly in men and women and most often occur in adults aged 15 to 40
Prevention:- For Adults;
Avoiding straining when defecation,
Careful anal hygiene after defection,
In case of pre-existing or suspected fissure, use of a lubricating ointment,
In infants, frequent diaper change can prevent anal fissure
Treatment:- Non- surgical treatment are recommended initially for acute and choric anal fissures. These include topical Nitroglycerin or calcium channel blockers or injection of Butulinum toxin into the anal sphincter
Other measures include warm Sitz baths, topical anesthetics, high fiber diet and stool softerners
Medication:-
Local application of medication to relax the sphincter muscle, thus allowing the healing to proceed, with Nitroglycerine ointment
Calcium channel blocker with Nifedipine ointment
A combined surgical and pharmacological treatment, administered by colorectal surgeons, is direct injection of Botulinum toxin(Botox) into the anal sphincter to relax it.
Surgery:-
1) Lateral internal sphincterotomy
2) Anal dilation
3) Stretching
DEFINITION
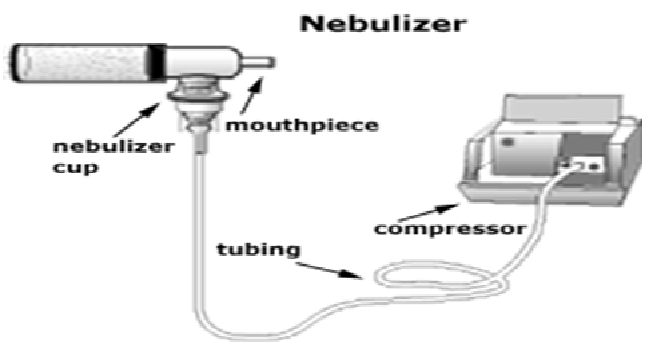
Nebulization is the process of medication administration via inhalation. It utilizes a nebulizer which transports medications to the lungs by means of mist inhalation.
INDICATION
Nebulization therapy is used to deliver medications along the respiratory tract and is indicated to various respiratory problems and diseases such as:
• Broncho-spasms
• Chest tightness
• Excessive and thick mucus secretions
• Respiratory congestions
• Pneumonia
CONTRAINDICATIONS
In some cases, nebulization is restricted or avoided due to possible untoward results or rather decreased effectiveness such as:
• Patients with unstable and increased blood pressure
• Individuals with cardiac irritability (may result to dysrhythmias)
• Persons with increased pulses
• Unconscious patients (inhalation may be done via mask but the therapeutic effect may be significantly low)
EQUIPMENTS
• Nebulizer and nebulizer connecting tubes
• Compressor oxygen tank
• Mouthpiece/mask
• Respiratory medication to be administered
• Normal saline solution
PROCEDURE
1. Position the patient appropriately, allowing optimal ventilation.
2. Assess and record breath sounds, respiratory status, pulse rate and other significant respiratory functions.
3. Teach patient the proper way of inhalation:
o Slow inhalation through the mouth via the mouthpiece
o Short pause after the inspiration
o Slow and complete exhalation
o Some resting breaths before another deep inhalation
4. Prepare equipments at hand
5. Check doctor’s orders for the medication, prepare thereafter
6. Place the medication in the nebulizer while adding the amount of saline solution ordered
7. Attach the nebulizer to the compressed gas source
8. Attach the connecting tubes and mouthpiece to the nebulizer
9. Turn the machine on (notice the mist produced by the nebulizer)
10. Offer the nebulizer to the patient, offer assistance until he is able to perform proper inhalation (if unable to hold the nebulizer [pediatric/geriatric/special cases], replace the mouthpiece with mask.
COMPLICATIONS
Possible effects and reactions after nebulization therapy are as follows:
• Palpitations
• Tremors
• Tachycardia
• Headache
• Nausea
• Broncho-spasms (too much ventilation may result or exacerbate Broncho-spasms)
• TEACHINGS
As nurses, it is important that we teach the patients the proper way of doing the therapy to facilitate effective results and prevent complications (demonstration is very useful). Emphasize compliance to therapy and to report untoward symptoms immediately for apposite intervention.
Auscultatory gap is the temporary disappearance of sounds normally heard over the brachial artery when the cuff pressure is high and the reappearance of the sounds at a lower level.
Provide excellent clues to the physiological functioning of the body.
• Alterations in body flexion are reflected in the body temp, pulse, respirations and blood pressure.
• These data provide part of the baseline info from which plan of care is developed.
• Any change from normal is considered to be an indication of the person’s state of health.
Author:PINKY CHOUDHARY
Description :- Placenta Previa
Definition :- Its is type of ante-partum hemorrhage. When the placenta is implanted partially or completely over the lower uterine segment , it is called Placenta previa.
Etiology :-
(1) The exact cause of implantation of placenta is unknown .
(2) Dropping Down Theory
(3) Persistence of chorionic activity in deciduas capsularis
(4) Big surface area of placenta
(5) Multiparity
(6) Increase maternal age
(7) History of previous cessarion section or scar in uterus
(8) Prior curettage use
Types :- There are four types of placenta previa .
(1) Type 1st( low lying ) – Major part of placenta is attached to upper segment & only margin reach on to lower segment but not up to os.
(2) Type 2nd (marginal ) – Placenta reach to margin of internal os but doesn’t cover it .
(3) Type 3rd ( Incomplete or partial central ) – Placenta cover the internal os partially .
(4) Type 4th (central or total ) – Placenta completely cover the internal os .
Clinical Features :- (1) Vaginal Bleeding
(2) Bleeding painless
(3)Bleeding is causeless & recurrent
(4) Anemic due to visible blood loss
Diagnosis :- –Sonography
–Magnetic resonance imaging
Management :- The following guidelines are useful to minimize the risk-
-Adequate antenatal care
– Antenatal diagnosis
– Significance of “Warning Hemorrhage ‘’ should not be ignored
Management at home :-
-Patients is immediately put to bed .
-To assess the blood loss .
-Note the pulse ,BP , & degree of anemia .
-Quick gentle abdominal examination .
-Vaginal examination must not be done .
Management in hospital :-
-Treatment depend on duration of pregnancy, fetal & maternal status & extend of hemorrhage .
-To give advice to pts for supplement therapy .
– Encourage the pts for steroid therapy .
– Vaginal delivery would be considered only in type 1& 2 placenta previa .
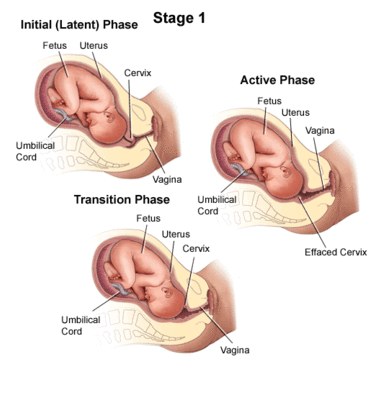
Definition:- Labour is called prolonged when the combined duration of first and second stage is more than 18 hours.
Labour is considered prolonged when cervical dialation rate is less than 1cm/hr.
Cause:-
a. First Stage:- Failure to dilate cervix
-Fault in power (abnormal uterine contraction)
-Fault in passage (contracted pelvis)
-Fault in passenger.
-Other (injudious admn. of analgesic)
b. Second Stage:-
-non descend of presenting part is due to failure in power( inability in bearing down, uterine inertia, epidural analgesia, constriction ring), fault in passage , fault in passenger.
Diagnosis:- prolonged labour has not diagnosis but it can be manifestated as abnormal. The cause of this prolonged labour can be detected by abdominal and vaginal examination.
First Stage:- first stage is considered prolonged when duration is more than 12 hrs. The rate of cervical dilatation is less than 1cm/hr in a primi and less than 1.5cm/hr in multi.
Second stage :- second stage is considered as prolonged when it is more than 2hrs in primi and more than 1hr in multi.
Diagnosis features are :-
Sluggish descending of presenting part
Variable degrees of moulding and caput formation in cephalic presentation.
Management:-
Prevention:- Antenatal or early intra-natal detection of the factors which produce prolonged labour.
Use of partograph, help early detection.
Selective and judicious augmentation of labour.
Change of posture in labour other than supine to increase uterine contraction
When progress is slow attempt should be made to determine the cause before deciding on management for insufficient uterine action is to encourage ambulation to produce normal activity.
The upright position for mother improve the application of the presenting part on to the cervix,this would make the contractions less painful but stronger and more efficient.
Adequate analgesic should be given to mother.
All observation are to be recorded on partogram.
The mother should be encouraged to empty the bladder about 2hrly.
Feotal Heart rate should be monitored.
Jishu Baiju